Pay Your Bill
Pay Your Bill in Person - Patient Accounts Office
Mason Health wants you to understand your hospital bill. If you have any questions please call (360) 427-3601; from Allyn call (360) 275-8614 and ask for the Patient Accounts Office. A Spanish interpretation services are available. Mason Health's online billpay services are powered by RevSpring™. Note: Do not save this link to your desktop or web browser, as it could be updated without warning.
ADDRESS
2505 Olympic Hwy, Suite #450 Shelton, WA 98584
CUSTOMER SERVICE HOURS
Monday - Friday: 8 a.m. - 4:30 p.m.
Please contact us by phone or email us at hospitalbillingquestions@masongeneral.com for assistance.
The Patient Accounts Office is open to the public. Safety precautions are in place and masking is required if you have symptoms of a respiratory illness.
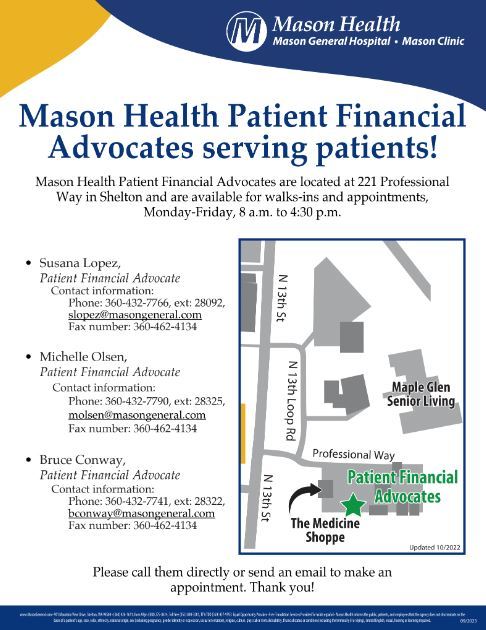
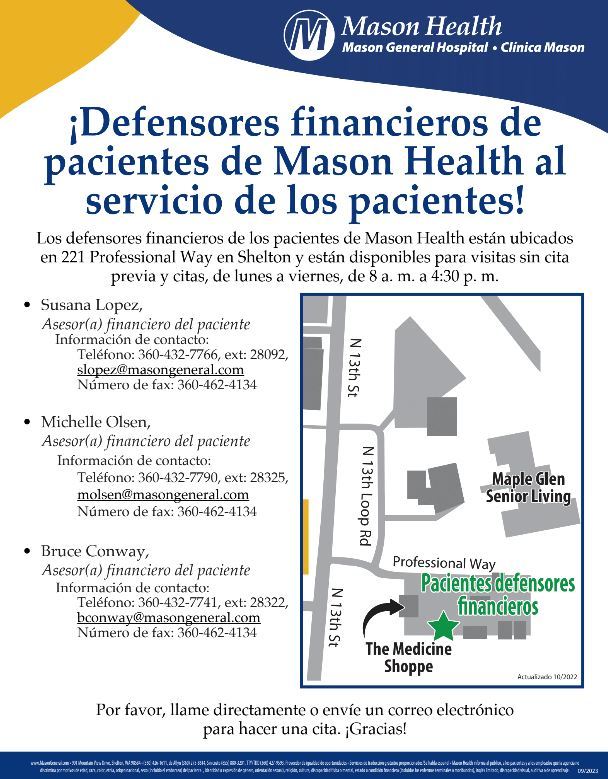
Need Help Paying Your Bill? Visit the Patient Financial Advocate Team
Disclosure of Healthcare Charges
Review the Disclosure of Healthcare Charges - Go to Disclosure of Healthcare Charges
Financial Assistance/Uncompensated Care
Mason Health has a Financial Assistance/Uncompensated Care Policy. This policy contains the guidelines for people to follow if they need any assistance with payment of their hospital bills. This policy applies to those who do not have insurance AND those who have insurance, and is based on income levels. Please ask at the Admitting area or the Business Office for a copy of the guidelines and an application. Completed applications should be sent or delivered to the Business Office.
Hospitals which are nonprofit and recognized as 501(c)(3) organizations (including Public Hospital District No. 1 of Mason County) shall limit amounts charged for emergency or other medically necessary care provided to individuals eligible for assistance under this Financial Assistance Policy to not more than the amounts generally billed to individuals who have insurance covering such care and may not collect “gross charges” from such individuals. See requirements WAC 246-453-040 and WAC 246-453-050 and IRS 501(r). This financial assistance update is effective for dates of service beginning January 1, 2016. Elective services are not covered under our Financial Assistance Policy or the 501(r) requirements.
Our Financial Assistance/Uncompensated Care Program is based on a sliding fee schedule extending up to 400% of the federal poverty level. In order to qualify you need to do three things:
- Complete the Financial Assistance/Uncompensated Care application
- Provide information about your family's gross income (income before tax deductions)
- Sign and date application
After all the criteria have been met, a determination will be made based on the income information.
Credit Policy
Mason Health recognizes the challenging times we are all facing. We are available to speak with you and can assist you with your bill. Please reach out to us if you have any questions or concerns. Financial arrangements should be made prior to admission for any pre-scheduled services. A deposit will be requested for services as appropriate. For those with insurance coverage, co-payments and deductibles will be requested at the time of service. If payment arrangements are needed, we ask that they are set up within 15 days from the date of service; whenever the bill cannot be paid in full at the time of the first billing statement. The account guarantor is responsible for making appropriate financial arrangements with the Business Office.
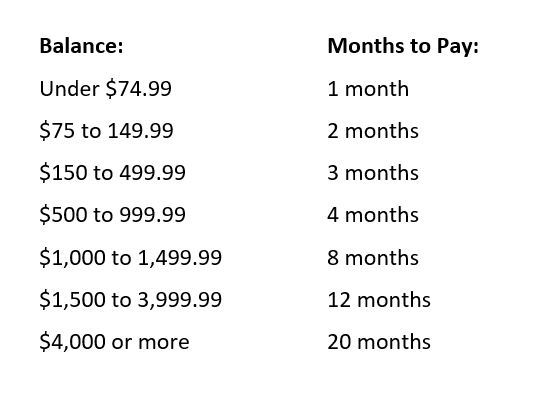
If payment arrangements are needed, the payment schedule is as follows:
Workman’s Compensation
For services that are the result of a work related injury the Business Office will need the following information:
- Employer name, address and phone number
- Date of injury
- Claim number, if applicable
You must notify your employer of an on-the-job injury. Your employer will need to submit additional information to the industrial carrier. Mason General Emergency Room physicians cannot help you with reopening a closed claim. You will need to go to your primary care physician for this service.
Auto Insurance
For services related to a motor vehicle accident, the Business Office will submit a bill on your behalf once the following information is received:
- The name of the responsible party
- The name and phone number of the responsible party's insurance carrier and agent's name
- The guarantor's auto insurance company name, phone number, and Agent name
- Any claim numbers assigned to you for this particular accident
Mason Health will not wait for litigation with regard to an accident. It will be your responsibility to pay the bill in a timely manner if insurance does not pay timely.
Insurance Information
Mason Health will bill your insurance company if all needed information and a copy of your insurance card is presented at the time of registration. At the time of registration, you will be asked to sign a form authorizing your insurance company to assign insurance benefits to Mason Health. You are expected to pay for charges that are not covered by insurance such as co-payment, coinsurance, non-covered and deductible amounts. Questions regarding insurance coverage or benefits must be directed to your insurance company. Is it your responsibility to know and meet the requirements of your insurance policy for pre-approval of your hospital service(s).
Contracted Payors
As of January 1, 2025, Mason Health is currently fully contracting and in-network with the following payors/insurers:
Commercial Plans:
- Aetna
- Cigna
- Community Health Plan of Washington (Cascade Select Individual Product)
- Coordinated Care (Ambetter Commercial Exchange Product)
- Excludes Cascade Care SELECT plan; non-contracted with no OON benefits
- First Choice Health Network
- Humana/ChoiceCare
- Kaiser Foundation Health Plan of Washington (PPO, POS and HMO)
- Premera BlueCross
- Regence BlueShield (includes Uniform Medical Plan)
- UnitedHealthcare
Medicaid:
- Community Health Plan of Washington (CHPW)
- Coordinated Care
- Molina Healthcare
- UnitedHealthcare
- Washington State Apple Health/HCA
- Wellpoint (formerly Amerigroup)
Medicare:
- AARP/UnitedHealthcare - Including Dual Eligible Special Needs Program/DSNP, PEBB Retirees and AT&T retiree program
- Community Health Plan of Washington Dual Eligible Special Needs Program/DSNP
- Humana/ChoiceCare Medicare Advantage
- Kaiser Medicare Advantage
- Molina Medicare Dual Eligible Special Needs Program/DSNP
- WellCare (Centene/Coordinated Care subsidiary) – Including Dual Eligible Special Needs Program/DNSP
- Wellpoint (Amerigroup) Dual Eligible Special Needs Program/DSNP
- Noridian/CMS
Other Payors:
- Labor & Industries
- US Family Healthplan/PacMed (TRICARE alternative)
- TriWest CCN/VA (network administered by Regence)
- TriWest TRICARE
- Opticare Vision
- EyeQuest Vision
- VSP Visioncare (for Molina Healthcare and Regence UMP PEBB enrollees only)
- InterWest Health Vision
If you have questions relating to a provider’s preferred, participating, network or non-network status, please refer those questions to your insurance company. The patient is responsible for meeting the requirements of their insurance policy and all questions regarding insurance coverage or benefits must be directed to your insurance company.
**No one will be denied services based on inability to pay. Discounts are available based on family size and income.**
Medicare Advantage Updates for 2025
At Mason Health we are communicating about some important information about Mason County Medicare Advantage plans for 2025. The Medicare Open Enrollment period for 2025 started October 15, 2024, and ends on December 7, 2024.
Mason Health (Mason General Hospital, Mason Clinic and Mason Clinic Hoodsport) continues to participate in the traditional Medicare program. General Medicare information is available at 800-633-4227 and at www.Medicare.gov.
In addition to traditional Medicare, Mason Health also has agreements with and will be fully in-network for the following Medicare Advantage plans in 2025 (in-network means your patient out-of-pocket cost may be lower for the service):
- AARP Medicare Advantage from UHC (UnitedHealthcare)
- PEBB Retiree Plan UnitedHealthcare
- Kaiser Permanente Medicare Advantage
- Humana Medicare Advantage
- WellCare Medicare Advantage
Several 2024 Medicare Advantage plans who are in Mason County in 2024 are not serving our county in 2025. Medicare’s annual open enrollment can be difficult at times, so we encourage you to reach out for assistance if needed. Senior Services for the South Sound runs our local State Health Insurance Benefits Advisors (SHIBA) program for Mason County. SHIBA volunteers are available at 360-586-6181. They are trained experts and can answer your questions or schedule an appointment to assist you. We suggest that you contact SHIBA first.
For questions regarding this letter or services offered at Mason Health, you may contact our In-Person Assistors at 360-427-3601, option 3. Please note that due to federal government regulations, Mason Health is not allowed to answer questions about specific plans or make plan recommendations.
To learn more about important Medicare Advantage Updates for 2025 - Please read this letter. This document is also available in the Downloads section below.
Para obtener más información sobre actualizaciones importantes de Medicare Advantage para 2025, lea esta carta. Este documento también está disponible en la sección Descargas a continuación.
Good Faith Estimate
You have the right to receive a “Good Faith Estimate” explaining how much your medical care will cost.
Under the law, health care providers need to give patients who don’t have insurance or who are not using insurance an estimate of the bill for medical items and services.
• You have the right to receive a Good Faith Estimate for the total expected cost of any non-emergency items or services. This includes related costs like medical tests, prescription drugs, equipment, and hospital fees.
• Make sure your health care provider gives you a Good Faith Estimate in writing at least 1 business day before your medical service or item. You can also ask your health care provider, and any other provider you choose, for a Good Faith Estimate before you schedule an item or service.
• If you receive a bill that is at least $400 more than your Good Faith Estimate, you can dispute the bill.
• Make sure to save a copy or picture of your Good Faith Estimate.
For questions or more information about your right to a Good Faith Estimate, email goodfaithestimate@masongeneral.com or you can visit www.cms.gov/nosurprises or call 1-800-985-3059.
Balanced Billing
When you see a doctor or other health care provider, you may owe certain out-of-pocket costs, such as a copayment, coinsurance, and/or a deductible. You may have other costs or have to pay the entire bill if you see a provider or visit a health care facility that isn’t in your health plan’s network.
“Out-of-network” describes providers and facilities that haven’t signed a contract with your health plan. Out-of-network providers may be permitted to bill you for the difference between what your plan agreed to pay and the full amount charged for a service. This is called “balance billing.” This amount is likely more than in-network costs for the same service and might not count toward your annual out-ofpocket limit.
“Surprise billing” is an unexpected balance bill. This can happen when you can’t control who is involved in your care—like when you have an emergency or when you schedule a visit at an in-network facility but are unexpectedly treated by an out-of-network provider.
Insurers are required to tell you, via their websites or on request, which providers, hospitals and facilities are in their networks. Hospitals, surgical facilities and providers must tell you which provider networks they participate in on their website or on request.
You are protected from balance billing for:
Emergency Services
If you have an emergency medical condition and get emergency services from an out-of-network provider or facility, the most the provider or facility may bill you is your plan’s in-network cost-sharing amount (such as copayments and coinsurance). You can’t be balance billed for these emergency services. This includes services you may get after you’re in stable condition, unless you give written consent and give up your protections not to be balanced billed for these post-stabilization services.
Certain services at an in-network hospital or ambulatory surgical center
When you get services from an in-network hospital or ambulatory surgical center, certain providers there may be out-of-network. In these cases, the most those providers may bill you is your plan’s in-network cost-sharing amount. This applies to emergency medicine, anesthesia, pathology, radiology, laboratory, neonatology, surgeons and assistant surgeons, hospitalists, or intensivist services. These providers can’t balance bill you and cannot ask you to give up your protections not to be balance billed.
If you get other services at these in-network facilities, out-of-network providers can’t balance bill you, unless you give written consent and give up your protections.
You’re never required to give up your protections from balance billing. You also aren’t required to get care out-of-network. You can choose a provider or facility in your plan’s network.
When balance billing isn’t allowed, you also have the following protections
- You are only responsible for paying your share of the cost (like the copayments, coinsurance, and deductibles) that you would pay if the provider or facility was in-network. Your health plan will pay out-of-network providers and facilities directly.
- Your health plan generally must:
- Cover emergency services without requiring you to get approval for services in advance(prior authorization).
- Cover emergency services by out-of-network providers.
- Base what you owe the provider or facility (cost-sharing) on what it would pay an in-network provider or facility and show that amount in your explanation of benefits.
- Count any amount you pay for emergency services or out-of-network services toward your deductible and out-of-pocket limit.
If you believe you’ve been wrongly billed, you may file a complaint with the federal government at https://www.cms.gov/nosurprises or by calling 1-800-985-3059; and/or file a complaint with the Washington State Office of the Insurance Commissioner at their website or by calling 1-800-562-6900.
Information in other languages:

Please visit the Office of the Insurance Commissioner website for information in other languages about the Federal No Surprises Act: CLICK HERE.



